Orthopedic therapy is a specialized form of physical therapy that focuses on the treatment of musculoskeletal conditions and injuries. It aims to improve the function and mobility of the musculoskeletal system, which includes the bones, joints, muscles, ligaments, and tendons. Orthopedic therapy is commonly used to treat conditions such as fractures, sprains, strains, tendonitis, bursitis, arthritis, and post-surgical rehabilitation. It is also beneficial for individuals with chronic pain or mobility issues related to musculoskeletal problems.
Orthopedic therapy differs from other forms of physical therapy in its specialized focus on musculoskeletal conditions. While general physical therapy may address a wide range of conditions, orthopedic therapy specifically targets issues related to the musculoskeletal system. Orthopedic therapists have advanced knowledge and training in diagnosing and treating orthopedic conditions, allowing them to provide more targeted and effective treatment plans. They may use a variety of techniques and modalities that are specific to orthopedic therapy to address the unique needs of their patients.
There are several common orthopedic injuries that may require therapy. These include fractures, which may require therapy to regain strength and mobility after the bone has healed. Sprains and strains, which are common injuries to ligaments and muscles, can also benefit from orthopedic therapy to reduce pain, improve range of motion, and prevent further injury. Tendonitis, an inflammation of the tendons, and bursitis, an inflammation of the fluid-filled sacs that cushion the joints, are other conditions that may require orthopedic therapy for pain relief and improved function. Additionally, individuals with arthritis or those who have undergone orthopedic surgery may also benefit from orthopedic therapy to manage pain and regain mobility.

Orthopedic therapy utilizes a variety of techniques and modalities to address musculoskeletal conditions. These may include manual therapy techniques such as joint mobilization, soft tissue mobilization, and myofascial release to improve joint mobility and reduce pain. Therapeutic exercises are also commonly used to strengthen muscles, improve flexibility, and restore normal movement patterns. Modalities such as heat or cold therapy, electrical stimulation, ultrasound, and laser therapy may be employed to reduce pain, inflammation, and promote tissue healing. Orthopedic therapists may also provide education on proper body mechanics and ergonomics to prevent further injury and promote long-term musculoskeletal health.
The duration of orthopedic therapy can vary depending on the individual and the severity of their condition. In general, orthopedic therapy may last anywhere from a few weeks to several months. The frequency and duration of therapy sessions will be determined by the therapist based on the specific needs of the patient. It is important to note that orthopedic therapy is often a progressive process, with the therapist gradually increasing the intensity and complexity of the exercises and treatments as the patient progresses.

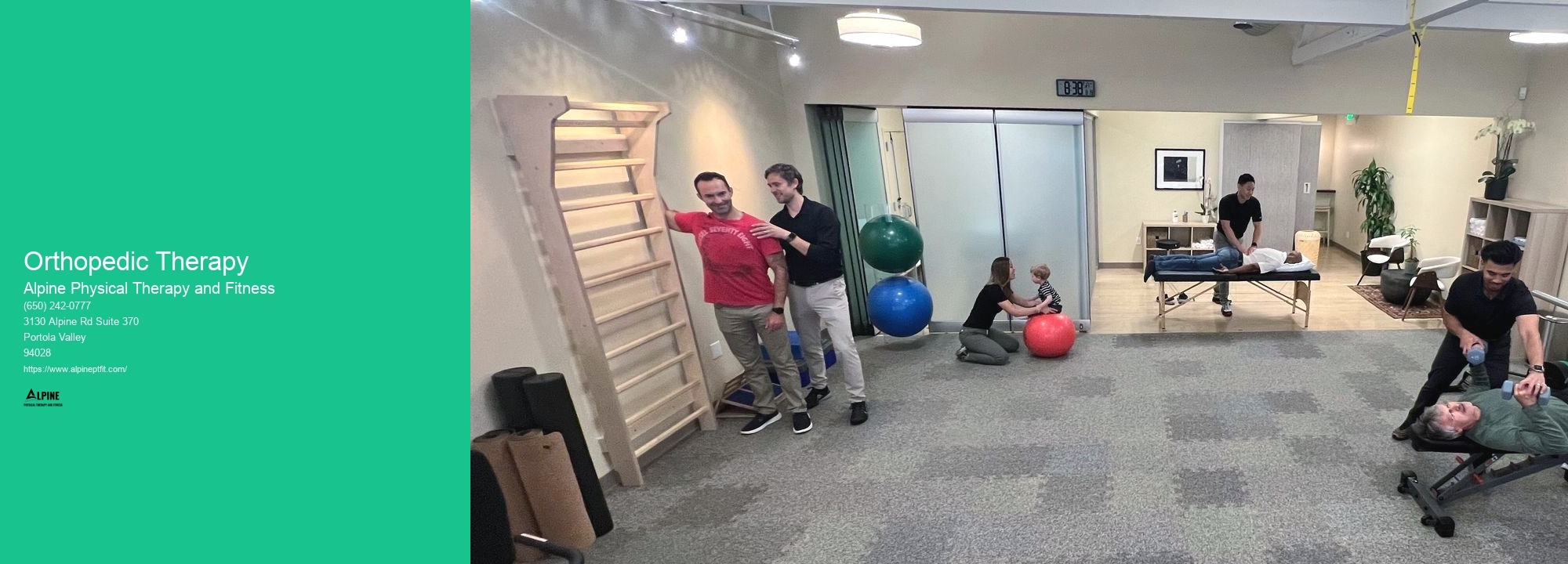
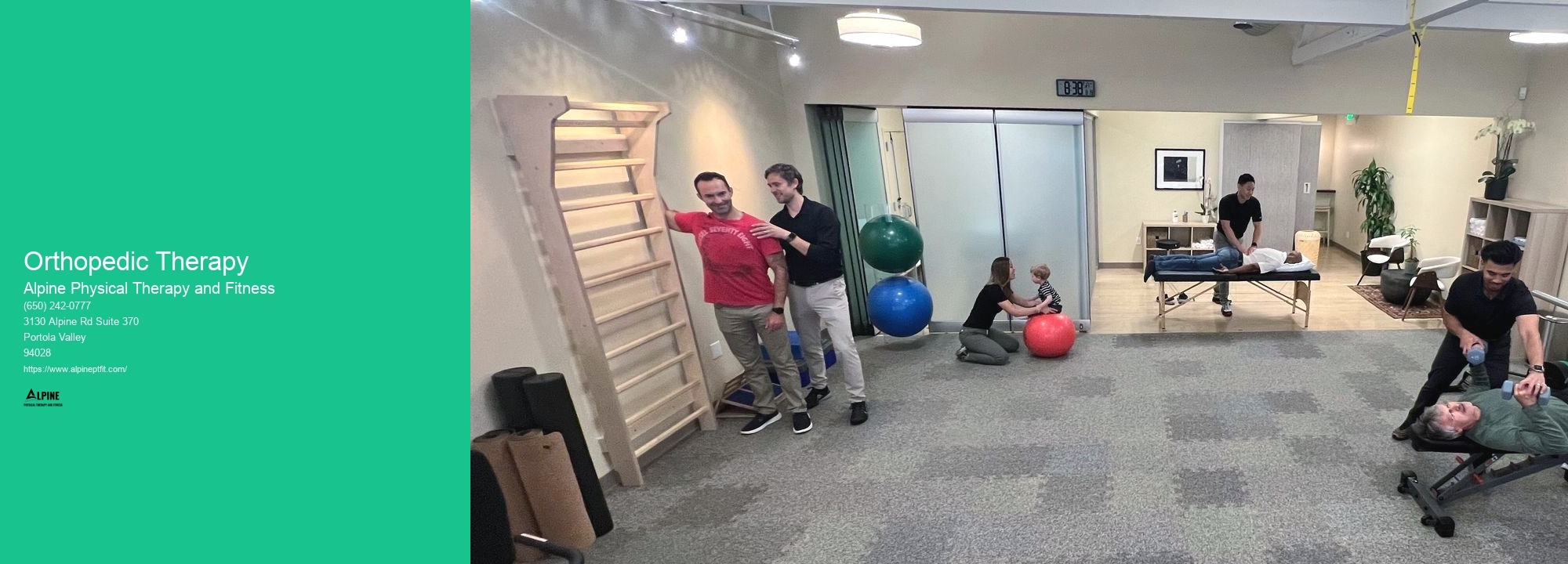
During an orthopedic therapy session, patients can expect a comprehensive evaluation of their condition by the therapist. This may involve assessing their range of motion, strength, flexibility, and any areas of pain or dysfunction. Based on the evaluation, the therapist will develop an individualized treatment plan that may include a combination of manual therapy techniques, therapeutic exercises, and modalities. The therapist will guide the patient through the exercises and treatments, providing hands-on assistance and guidance as needed. They will also educate the patient on proper techniques and exercises to continue at home to support their recovery.
While orthopedic therapy is generally safe, there are some potential risks and side effects to be aware of. In rare cases, certain manual therapy techniques or exercises may cause temporary discomfort or soreness. However, these side effects are typically mild and transient. It is important for patients to communicate any concerns or discomfort they may experience during therapy sessions to their therapist. Additionally, individuals with certain medical conditions or who are taking certain medications may need to take precautions or modify their therapy program. It is important to consult with a healthcare professional before starting orthopedic therapy to ensure it is safe and appropriate for your specific situation.

Physical therapy has been shown to be effective in improving mobility and function in older adults with frailty. Frailty is characterized by a decline in physical function and increased vulnerability to stressors. Physical therapy interventions, such as strength training, balance exercises, and gait training, can help improve muscle strength, balance, and coordination, which are essential for maintaining mobility and function. Additionally, physical therapy can also address specific impairments, such as joint stiffness or muscle weakness, through targeted interventions. By addressing these physical limitations, physical therapy can help older adults with frailty regain independence, reduce the risk of falls, and improve overall quality of life.
The principles of rehabilitation for a baseball pitcher with shoulder issues involve a comprehensive approach that focuses on restoring strength, flexibility, and stability to the shoulder joint. The rehabilitation program typically includes a combination of exercises, manual therapy techniques, and modalities such as heat or ice therapy. Specific exercises may include rotator cuff strengthening exercises, scapular stabilization exercises, and range of motion exercises. It is important to gradually progress the intensity and volume of the exercises to avoid overloading the shoulder. Additionally, proper throwing mechanics and technique should be emphasized to prevent further injury. The rehabilitation process may also involve addressing any underlying biomechanical issues or muscle imbalances that may have contributed to the shoulder issues. Overall, the goal of rehabilitation is to not only alleviate pain and restore function but also to prevent future injuries and optimize performance.
The goals of physical therapy in improving lung function after lung surgery are to enhance respiratory muscle strength, increase lung capacity, improve oxygenation, promote effective coughing and deep breathing, and enhance overall physical endurance. Physical therapists utilize various techniques such as breathing exercises, chest physiotherapy, and aerobic conditioning to achieve these goals. By targeting specific muscles involved in respiration and implementing exercises that promote deep breathing and effective coughing, physical therapy can help patients regain optimal lung function and improve their overall quality of life.
The most common physical therapy interventions for treating tennis elbow include a combination of exercises, manual therapy techniques, and modalities. Exercises often focus on strengthening the muscles of the forearm and improving flexibility. These may include wrist curls, forearm pronation and supination exercises, and eccentric exercises. Manual therapy techniques such as soft tissue mobilization and joint mobilization can help reduce pain and improve range of motion. Modalities such as ultrasound, electrical stimulation, and ice or heat therapy may also be used to reduce inflammation and promote healing. Additionally, education on proper ergonomics and activity modification may be provided to prevent further injury and promote long-term recovery.
Physical therapy plays a crucial role in the management of temporomandibular joint (TMJ) disorders by providing targeted interventions to alleviate pain, improve jaw function, and enhance overall quality of life. Through a comprehensive assessment, a physical therapist can identify the specific impairments and functional limitations associated with TMJ disorders, such as limited jaw mobility, muscle imbalances, and joint inflammation. Based on this evaluation, a personalized treatment plan is developed, which may include a combination of manual therapy techniques, therapeutic exercises, and modalities. Manual therapy techniques, such as joint mobilizations and soft tissue mobilizations, aim to restore normal joint mechanics and reduce muscle tension. Therapeutic exercises focus on strengthening the muscles around the jaw, improving jaw stability, and promoting proper alignment. Additionally, modalities like heat or cold therapy, ultrasound, and electrical stimulation may be used to reduce pain and inflammation. By addressing the underlying causes of TMJ disorders and promoting optimal jaw function, physical therapy helps individuals regain pain-free jaw movement, improve chewing and speaking abilities, and ultimately enhance their overall well-being.
Patients with bursitis are recommended to engage in a variety of exercises that can help alleviate symptoms and promote healing. Low-impact exercises such as swimming, cycling, and walking are often suggested as they minimize stress on the affected joints. Strengthening exercises that target the muscles surrounding the affected area, such as leg lifts, squats, and lunges, can also be beneficial. Additionally, stretching exercises that focus on improving flexibility and range of motion, such as yoga or Pilates, may help reduce pain and inflammation. It is important for patients to consult with a healthcare professional or physical therapist to determine the most appropriate exercises for their specific condition and to ensure proper form and technique.